What is ULCERATIVE COLITIS?
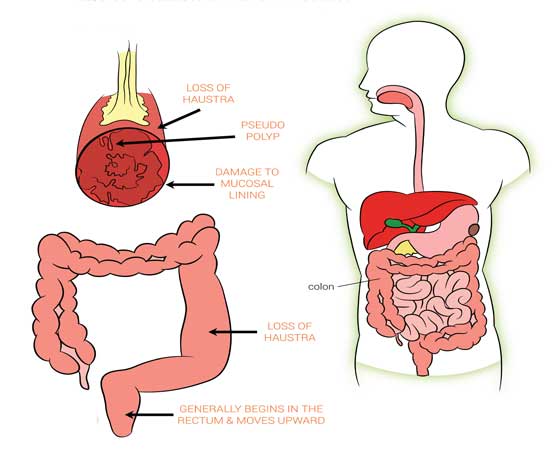
UC is a chronic autoimmune disease that causes inflammation and ulcers in the lining of the colon, or large intestine. The inflammation sometimes occurs only in the lower part of the colon and the rectum, but it may also affect the entire colon. Ulcerative colitis is a lifelong illness that has a profound emotional and social impact on the affected patients.
What causes UC?
Although the exact cause of inflammatory bowel diseases like UC is not yet known, extensive research has been conducted in this area and the disease appears to be multifactorial and polygenic. The proposed causes include environmental factors, immune dysfunction, and a likely genetic predisposition. It is believed that UC occurs when the patient's immune system inappropriately responds to something it perceives to be a foreign substance in the body (e.g., the bacteria normally found in the colon). Once triggered, this abnormal immune response leads to inflammation and intestinal damage.
Who is at risk?
Both men and women have an equal chance of developing UC, and it is known that genetics play a role in determining who is at greater risk. Although the disease usually develops between the ages of 15 and 30, UC can occur at any age. There are many factors involved with the disease. While it is believed that UC is not caused by emotional stress, food or drugs (like NSAID's, antibiotics), these factors may aggravate its symptoms.
What are the symptoms of UC?
Patients with ulcerative colitis predominantly complain of rectal bleeding, with frequent stools and mucous discharge from the rectum. Some patients also describe tenesmus (Severe urgency to have a bowel movement). Onset is typically insidious. In severe cases, purulent rectal discharge causes lower abdominal pain and severe dehydration, especially in the elderly population.
- Arthritis, which may involve the large joints (e.g., knee), or the spine. Spinal involvement may include a disease called ankylosing spondylitis, which is an important cause of disability.
- Skin disorders where painful nodules or deep ulcers may develop on the skin
- Increased risk for certain liver disorders, such as scarring of the bile ducts which can lead to liver diseases.
- Inflammation of the eye which can cause redness and pain and, rarely, lead to vision loss.
- Fatigue.
Other symptoms include
How is Ulcerative Colitis diagnosed?
Diagnosing UC involves a series of tests. Blood tests are performed to check for anemia (a low red blood cell count).
Often, an evaluation of the colon is performed using endoscopy - either a sigmoidoscopy, where the doctor passes a flexible instrument into the rectum and lower colon, or a colonoscopy, a similar procedure, which gives the doctor a visualization of the entire colon. Multiple biopsy samples are obtained from both inflamed and normal-appearing mucosa.
Radiographic imaging has an important role in the workup of patients with suspected inflammatory bowel disease and in the differentiation of ulcerative colitis and Crohn disease. Plain abdominal radiographs are a useful adjunct to imaging in cases of ulcerative colitis of acute onset. In severe cases, the images may show colonic dilatation, suggesting toxic megacolon; evidence of perforation; obstruction; or ileus.
Stool studies are used to exclude other causes of similar complaints. These include evaluation of fecal leukocytes, ova and parasite studies, culture for bacterial pathogens, and Clostridium difficile titer.
When should I talk to my doctor?
Whether or not you have been diagnosed with UC, you should consult a doctor if you experience any of its symptoms, including those listed below:
- Severe abdominal pain.
- Blood in your bowel movements
- Ongoing diarrhea
- Unexplained fever that lasts longer than a couple of days
What are the complications of UC?
- Bleeding: Rectal bleeding and bloody diarrhea are two of the hallmark symptoms of UC.
- Anemia: In UC, this is usually the result of chronic blood loss. To combat anemia, doctors often prescribe supplements, and recommend a diet rich in iron.
- Malnutrition: Symptoms such as diarrhea and rectal bleeding can lead to a loss of fluids and nutrients.
- Growth retardation: In children with UC, a combination of factors, including malnutrition and the use of corticosteroid treatment, may contribute to growth retardation.
- Osteoporosis: UC patients are at risk for low bone density, chiefly due to long-term use of some medications, such as steroids.
- Structures: Abnormal narrowing of the intestine due to swelling and scarring leads to obstruction of the lumen of the intestine.
- Hospitalization: Occurs when symptoms are too severe to control with medication.Hospitalization is required to stop diarrhea, loss of fluids, blood, or nutrients. In some cases,surgery may be required at this point.
- Toxic megacolon: This serious complication may occur when inflammation spreads from the lining of the colon to involve the entire intestinal wall. Because this involvement temporarily stops the normal contractile movements of the intestine, the large intestine may greatly expand. The person is usually severely ill with fever, abdominal pain and distension.Immediate and aggressive measures are required to minimize risk of death.
- Perforation: Extensive inflammation can lead to a tear in the intestinal wall, resulting in leakage of bowel contents outside the intestine. Categorized by sudden, severe abdominal pain, shock, and excessive abdominal tenderness, this condition usually requires emergency surgery.
- Colon cancer: UC patients have a higher risk of developing colon cancer. The risk increases when a greater proportion of the colon is affected, or if a patient has had UC for a prolonged period of time. Gastroenterologists may recommend that certain UC patients undergo periodic screening for colon cancer, based on disease duration.
UC Treatment Options
The treatment of ulcerative colitis relies on initial medical management with corticosteroids and antiinflammatory agents, such as sulfasalazine, in conjunction with symptomatic treatment with antidiarrheal agents and rehydration. Surgery is contemplated when medical treatment fails or when a surgical emergency (eg, perforation of the colon) occurs. Surgical options include total colectomy (panproctocolectomy) and ileostomy, total colectomy, and ileoanal pouch reconstruction or ileorectal anastomosis.
While there are a variety of drugs currently used to treat the symptoms of UC, there remains an unmet medical need. The location and severity of your disease, specific complications, and your response to previous treatment will all influence the choice of therapy.The current treatment options include:
- Aminosalicylates (5-ASA agents): Drugs such as sulfasalazine are used to reduce the inflammation of UC and to prevent flare-ups. These drugs are usually taken orally, although they may also be given rectally as enemas. They are usually well-tolerated, but possible side effects of mesalamine preparations include nausea, vomiting, heartburn, diarrhea, and headache. These drugs are effective in treating mild to moderate UC, and are also useful in preventing disease relapse.
- Biologics: Biologics are the latest form of therapy being used to treat ulcerative colitis. These treatments work by targeting an underlying cause of inflammation that leads to the painful and unpredictable symptoms characteristic of ulcerative colitis.To date, biologics have been used to successfully treat many people with different types of inflammatory disorders. These include Infliximab, Adalimumab, Certolizumab, Natalizumab, Vedolizumab etc.
- Immunomodulators: Drugs such as azathioprine have been used to maintain remission and decrease the need for steroids. However, this class of drugs may take up to 2-4 months to produce their maximal effect. One may experience side effects such as nausea, vomiting, and diarrhea, as well as low white blood count, liver problems, pancreatitis and reduced resistance to infection. So persons on these drugs need to have their blood count monitored on a regular basis. Cyclosporine has been given to some people who are having severe flare-ups not responsive to corticosteroid therapy
- Steroids: Corticosteroids are usually given to patients with moderate to severe disease. Prednisone is often used to control the inflammation of UC, followed by sulfasalazine, olsalazine, or mesalamine to maintain remission. Because of the many side effects that may occur with steroid treatment, it is tried to wean off this therapy as quickly as possible.
- Antidiarrheal medications: Antidiarrheal agents may be prescribed. In severe cases, these may trigger toxic megacolon. If one is dehydrated because of diarrhea, he/she will be treated with fluids and electrolytes.
What is the role of surgery?
Surgery may be required to provide relief for patients who have not responded to medical treatment or whose health has been threatened by bleeding, severe illness, rupture of the colon or other complications of treatment. In addition, surgery is required when colon cancer or dysplasia, a condition that precedes it, develops. Removing the colon is called a colectomy and may be performed in 5-10% of patients.
Two common surgical procedures are:
- Ileostomy: During this procedure, the surgeon creates a small opening in the abdomen, called a stoma, and attaches the end of the small intestine, called the ileum, to it. The stoma is about the size of a quarter and is covered by a pouch. Waste travels through the small intestine and exits the body through the stoma and into the pouch. The patient empties the pouch as needed.
- Ileoanal anastomosis: This is a procedure that allows the patient to have bowel movements via the normal route because the small intestine is connected to the anus. The colon is still removed but the doctor creates an internal pouch from the small bowel and attaches it to the anus. Waste is stored in the pouch and passed through the anus in the usual manner.
- Small bowel obstruction: A blockage in the small bowel can cause nausea, vomiting, cramps and abdominal pain. Approximately one-third of those who experience this complication require surgery to release the bowel from the source of obstruction. The obstruction is usually caused by scar tissue that forms in the abdominal cavity after surgery, called an adhesion.
- Pouchitis: At least 30% of people who have received the ileoanal pouch develop inflammation, called pouchitis. The symptoms of pouchitis include frequent bowel movements and/or diarrhea. These symptoms can be mild or severe, acute or chronic. Some patients require long-term antibiotics to manage this condition.
- Pouch failure: Approximately 8-10% of patients develop pouch failure Unlike pouchitis,failure requires that the pouch be removed and necessitates a switch to a permanent ileostomy.
As with any surgical procedure, complications may arise. Common long-term complications include:
© Copyright 2022- All Rights Reserved. Designed by Harksh Technologies
