What is Crohn's disease?
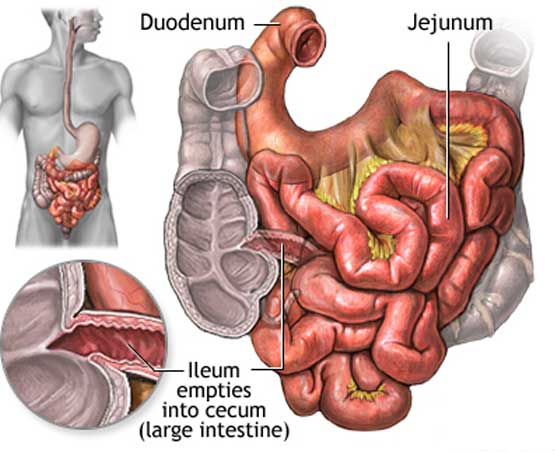
Crohn's disease is a chronic inflammatory disorder that causes inflammation of the digestive tract. It can affect any area of the GI tract, from the mouth to the anus, but it most commonly affects the lower part of the small intestine, called the ileum. It is believed to be the result of an imbalance between proinflammatory and anti-inflammatory mediators. Genetic susceptibility, intestinal microorganisms, and environmental triggers are important factors which induce intestinal inflammation, although no single factor alone can precipitate inflammation. Historically the disease was thought to be more common in western population, but more recently the incidence and prevalence of Crohn's disease is increasing in developing countries of Asia and Africa.
The disease occurs in two age groups. First in the age group of 15 and 30 years (late adolescence and early adulthood), and the second occurs mainly in women between the ages of 60 and 70 years.
What are the symptoms of Crohn's disease?
Clinical manifestations of Crohn's disease are variable. Symptoms may be present for many years before the diagnosis is made.Fatigue, prolonged diarrhea with abdominal pain and with or without gross bleeding, weight loss, and fever, are the hallmarks. The inflammation in Crohn's disease involves the deeper lining of the organs involved and some people may also develop fistulizing Crohn's, in which the intestinal wall develops fistulas or tunnels that connect the intestine to adjacent areas, including the skin, bladder, vagina, intestine, and perianal areas.
- Loss of appetite
- Ulcers in oral cavity
- Difficulty in swallowing
- Sores around the anal area
- Joint pain
- Redness and pain in eyes
- Kidney stones
- Gall stones
- Skin rash
- Blockage in large arteries and veins
- Bronchitis
Other symptoms of Crohn's include:
Conditions with similar symptoms
Sometimes other conditions can cause abdominal symptoms that appear to be similar to those of Crohn's. These conditions include:
- Intestinal tuberculosis
- Ulcerative colitis
- Irritable bowel syndrome
- Appendicitis
- Diverticulitis
- Peptic ulcer disease
How is Crohn's disease diagnosed?
An accurate professional diagnosis is the first step in treating Crohn's. Proper diagnosis is particularly important with a condition like Crohn's, because its symptoms may mimic those of other conditions and its effects are chronic, progressing over time.
Diagnostic tests
To confirm the diagnosis — and to rule out other conditions that can cause similar symptoms, such as other inflammatory bowel diseases, colitis, celiac disease, or irritable bowel syndrome — a physician/gastroenterologist needs to do a thorough complete physical examination and perform some medical tests.
These diagnostic tests may include:- Blood tests: Although a complete blood count cannot provide a positive diagnosis of Crohn's, physicians usually order the test in suspected cases because it may reveal intestinal bleeding, an infection, or an inflammatory condition. These include Complete blood count (CBC), blood chemistry including electrolytes, renal function tests, liver enzymes , and blood glucose, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), serum iron and vitamin B12 levels etc.
- Endoscopic Examinations: These tests use a tool called an endoscope — a thin, flexible, lighted tube that is linked to a computer and video monitor. In an endoscopic exam, the endoscope is inserted into the rectum or mouth to give gastroenterologists a detailed view of the intestinal tract.
- Radiologic examinations: Imaging studies are most useful to evaluate the upper gastrointestinal tract and allow documentation of the length and location of strictures in areas which can not be assessed by endoscopy. Traditionally barium studies, such as barium enema or upper gastrointestinal series with SBFT were done, though the use of CT and magnetic resonance enterography (MRE) is becoming more standard of care in imaging in patients with CD
- Stool Tests: These noninvasive tests examine stool samples to determine whether a patient has Crohn's disease, ulcerative colitis, or a bacterial infection.
- Urine Tests: Also called urinalysis, these tests are used to detect the presence of bacteria, red blood cells, and white blood cells in your urine. When bacteria and white blood cell levels are raised, it may indicate a urinary tract infection, which can be a complication of Crohn's.
Different endoscopic exams may include:
• Sigmoidoscopy: This test is the most commonly performed endoscopic exam used to confirm a diagnosis of Crohn's. By using either a flexible or rigid instrument, a physician can evaluate the rectum and lower end of the colon for signs of inflammation.
• Colonoscopy: This test examines the full length of the colon, as well as the lower part of the small intestine.
• Upper endoscopy: In this exam, an endoscope is placed into a patient's mouth and guided through the stomach to the upper intestine.
• Enteroclysis: In this test, a tube is inserted into the nose and guided through the stomach to the duodenum, which is where the small intestine begins. A barium-based liquid is then infused through the tube, and x-rays are used to reveal abnormalities within the small intestine.
• Computerized tomography (CT) scan: This extremely precise x-ray is used to detect abnormalities in the liver, kidneys, and intestines after a dye is ingested, administered intravenously, or inserted through the rectum.
• Magnetic resonance imaging (MRI): By using radio waves and superconducting magnets, this test can help detect fistulas and abscesses within a person's body without exposure to radiation.
• Ultrasound: By using sound waves, this test examines organs of the pelvis and abdomen without exposure to radiation.
• Barium enema: This test helps physicians visualize the colon and rectum.
• Upper GI and small bowel follow-through: In this test, x-rays help examine the esophagus, stomach, duodenum, and small intestine after a patient drinks a barium-based liquid.
Is Crohn's disease curable?
Although there is no cure for Crohn's, the sooner Crohn's is diagnosed, the better the chances of managing its symptoms and avoiding potentially serious complications of the disease.
Who treats Crohn's disease?
In most cases, people with Crohn's disease are treated by a gastroenterologist. Sometimes your gastroenterologist may be an internist or family practitioner
Complications of Crohn's disease
The complications that Crohn's patients experience depend on the location and severity of the disease. Some complications can be life threatening, while others are manageable with the help of treatment plans prescribed by a gastroenterologist
Serious complications
Crohn's may cause serious complications, which can happen over the course of the illness:
- Obstruction: Obstructions can occur when the intestinal wall swells inward, reducing the capacity for fluids to flow through the intestine.
- Fistula: Sometimes ulcers caused by Crohn's will channel through the gut wall to adjacent areas, including the skin, bladder, vagina, intestine, and perianal areas. These occurrences are known as fistulas and may require medical or surgical therapy.
- Abscess: An abscess is a localized collection of bacteria that eventually accumulates pus and places painful pressure on adjacent tissues.
- Free perforation: A free perforation is the formation of a hole in the bowel wall that allows intestinal contents to enter the abdominal cavity.
- Hemorrhage: In rare cases, a bleeding ulcer may burrow through the gut wall and shear an artery. This produces a life-threatening hemorrhage that may require blood transfusions and special measures to promote blood clotting. Sometimes emergency surgery is required.
• A patient may experience painful cramps or vomiting due to food that is not able to bypass the obstruction.
• Patients who experience an obstructive episode are usually hospitalized and given intravenous fluids and salts to compensate for fluid losses.
• A fistula that tracks into the abdominal cavity may produce infection and form an abscess. Abscesses may also occur in the pelvic tissues or the perineum, if a fistula fails to drain.
• Abscesses can be difficult for gastroenterologists to diagnose; however, after they are located, they should be drained. This may require surgery.
• Patients are usually given a course of antibiotics to reduce the risk of further infection.
• Signs of free perforation include sudden, severe abdominal pain, shock, and excessive abdominal tenderness.
• The infection that results is called peritonitis and requires emergency surgery in which the leak is sealed and the abdominal cavity is cleansed to stop infection.
Other Chronic Complications
People with Crohn's may experience chronic or long-lasting complications that require ongoing management:
- Anemia: Anemia is a condition that results from lack of red blood cells.
- Malnutrition: Malnutrition occurs when the body does not receive enough nutrients to grow and develop properly.
• Anemia in Crohn's may be the result of chronic blood loss; bone marrow depression; or failure to absorb iron and folic acid, which are important in stimulating the production of red blood cells.
• Certain medications, such as sulfasalazine, may also exacerbate anemia. To combat most cases of anemia, gastroenterologists often prescribe supplements, and recommend a diet rich in iron.
• Loss of protein, tissue breakdown due to steroid use, poor diet and, in some cases, failure to absorb nutrients result in weight loss and nutritional deficiencies.
• Gastroenterologists often prescribe nutritional supplements to avoid the complications that result from deficiencies in vitamins A, D, E, and K.
Current Treatment Options
The general goals of treatment for Crohn disease are as follows:
• To achieve the best possible clinical, laboratory, and histologic control of the inflammatory disease with the least adverse effects from medication.
• To permit the patient to function as normally as possible.
• In children, to promote growth with adequate nutrition.
There are two general approaches to the outpatient treatment of Crohn disease: step-up therapy and top-down therapy. Step-up therapy typically starts with medications that are less potent and (often) associated with fewer side effects. If those therapies are ineffective, more potent (and potentially more toxic) medications are used. Top-down therapy starts with more potent therapies, such as biologic therapy or immunomodulator therapy, relatively early in the course of the disease. In general, we favor step-up therapy. Currently available treatments for Crohn's include:
- Anti-inflammatory medication: Most people who have Crohn's receive one or more different types of drugs designed to control inflammation. These may include sulfasalazine, other medications containing mesalamine (known as 5-ASA agents), and corticosteroids (Prednisolone, Budesonide, Methyl prednisolone, etc.) Budesonide is available in an ileal controlled-release form and is used for the treatment of ileal or right-side colonic disease.
- Immunosuppressive medication: These drugs block the body's immune response, which leads to inflammation. Immunosuppressive medications used to treat Crohn's include azathioprine, 6-mercaptopurine, methotrexate, and cyclosporine
- Biologics: Infliximab (REMICADE) is the first agent approved for moderate to severe Crohn's disease in adults and children who haven't responded well to other therapies. Adalimumab, Certolizumab, Natalizumab, Vedolizumab are the other biologicals available. These are useful for both inducing remission as well as maintenance of remission.
- Antibiotics: Antibiotics, such as metronidazole and ciprofloxacin, may help heal abscesses and fistulas. Other antibiotics may be prescribed to treat bacterial growth in the intestine caused by obstruction or abscesses.
- Antidiarrheal medication: Antidiarrheal medication offers some relief for the diarrhea that many people with Crohn's experience. Loperamide, codeine, and even fiber powders can help alleviate symptoms
- Nutritional supplements: Nutritional supplements are helpful for people who lose calories and nutrients from diarrhea or decreased appetite. Supplements can help fuel the body and replenish iron, calcium, other minerals, and vitamins.
- Surgery: If other treatments do not effectively control symptoms, your doctor may recommend surgery to close fistulas or remove the part of the intestine where the inflammation is most severe. Unfortunately, this procedure usually leads to only temporary remission of symptoms. The inflammation often returns near the area where the tissue was removed.
Some people may experience long periods of remission when they are free of symptoms. However, symptoms usually recur at various times over a person's lifetime. It is not possible to predict when a remission may occur or when symptoms will return. Because of the unpredictability of Crohn's, one may need medical care for long periods of time.
© Copyright 2022- All Rights Reserved. Designed by Harksh Technologies
